The Rising Cyber Risk in Healthcare
It’s no secret that healthcare is under a lot of pressure from cyber criminals. As hospitals and clinics embrace digital tools such as cloud-based records and even smart infusion pumps, they’ve opened the door to new cyber threats. And unlike in other sectors, when a system goes down here, it’s not just revenue on the line. It’s patients’ safety.
Why healthcare is a prime target:
- High-value data: Medical records fetch as much as value credit card numbers. They include personal info, insurance details, and sometimes even biometric data.
- Critical uptime: Attackers know healthcare can’t afford downtime. That makes ransomware a particularly effective and profitable weapon.
- Legacy systems: Many healthcare IT systems are outdated or lack proper segmentation, making them easy targets.
- Wider attack surface: With connected medical devices (IoMT), remote care platforms, and third-party vendors, entry points are multiplying.
Real-world wake-up calls:
- WannaCry (2017) shut down parts of the UK’s NHS, canceling thousands of appointments.
- Düsseldorf University Hospital (2020) faced a ransomware attack that disrupted emergency services—and may have contributed to a patient’s death.
The bottom line?
Cybersecurity in healthcare isn’t just about compliance anymore. It’s about resilience. A compromised server or hijacked EHR system can mean life or death. Healthcare leaders must stop treating cybersecurity as a back-office IT issue, and start treating it like the clinical risk it is.
What NIS2 Brings to the Table for Healthcare Providers
The NIS2 Directive is the EU’s way of saying: “Enough is enough. Cybersecurity is no longer optional.” For healthcare providers, this means a serious step up in expectations, accountability, and the way security is managed across the board.
What is NIS2, in plain terms?
It’s a major update to the original 2016 NIS Directive, aimed at strengthening the cybersecurity posture of essential and important entities across the EU. Healthcare, whether public hospitals, private clinics, or even digital health platforms, falls squarely into the “essential entities” category.
What does that mean for healthcare organizations?
- Stricter obligations: You now need to implement technical, operational, and organizational measures to manage cyber risks.
- Faster incident reporting: Major incidents must be reported to national authorities within 24 hours (initial) and 72 hours (detailed report).
- Board-level responsibility: Senior management can’t delegate cybersecurity to IT and call it a day. They’re now personally liable for ensuring compliance.
- Vendor vigilance: If your systems depend on external service providers (and let’s be honest, they probably do), you’re now expected to ensure their security too. Welcome to supply chain risk management.
- Enforcement with teeth: Non-compliance can lead to major fines, up to €10 million, or 2% of revenue.
Why does this matter for healthcare?
- Because cyber resilience is now tied to patient safety.
- Because delayed reporting in a ransomware attack can literally cost lives.
- And because the era of voluntary good practices is over. It’s time for legally binding standards and real accountability.
In short, NIS2 isn't a suggestion. It's a directive, and if you’re in healthcare, it’s your new reality.
CyberFundamentals – A Practical Blueprint for Cyber Hygiene
Let’s face it, many healthcare organizations don’t have the time, budget, or energy to implement something as heavyweight as ISO 27001 from scratch. That’s where CyberFundamentals comes in. Think of it as cybersecurity with training wheels.
What is CyberFundamentals?
Developed by Belgium’s Centre for Cybersecurity (CCB), CyberFundamentals is a tiered framework offering practical, actionable security controls. It’s designed for organizations that need guidance but don’t want to drown in standards and policies.
Even though it’s Belgian in origin, the principles apply far beyond Belgium, especially in healthcare environments that are struggling with resource constraints.
The 4 levels: Flexibility built in
CyberFundamentals is split into four assurance levels:
- Small – For organizations with low risk and minimal digital footprint.
- Basic – A foundational level that includes critical safeguards like MFA, backups, and patching.
- Important – Aimed at more complex organizations, like mid-sized clinics or regional hospital networks.
- Essential – For critical infrastructure operators, where uptime and data integrity are vital (think: national hospitals, large-scale providers).
Each level builds on the previous one, allowing healthcare orgs to scale their cybersecurity maturity over time, without feeling overwhelmed on day one.
Why healthcare should care:
- It’s practical: Instead of lengthy documentation, you get a checklist of controls that are achievable and relevant.
- It’s scalable: Start small, move up as your needs and risk exposure grow.
- It’s aligned: The framework syncs with international standards and maps well to NIS2 requirements (more on that in the next chapter).
- It speaks your language: Controls like “restrict admin rights” or “test backups” are far easier to apply than abstract ISO clauses.
Healthcare teams are busy saving lives. CyberFundamentals respects that. It gives them a way to improve cyber hygiene without disrupting clinical workflows or hiring an army of consultants.
Mapping CyberFundamentals to NIS2 Requirements in Healthcare
Let’s connect the dots. You’ve got NIS2, which lays out the “what” of cybersecurity compliance. Then you’ve got CyberFundamentals, which gives you the “how”, in plain language. When you put them together, you get a realistic, scalable approach to building cyber resilience in healthcare.
So how do they align?
NIS2 requires healthcare organizations to implement measures across key domains. Here's how CyberFundamentals helps you hit those marks:
| NIS2 Domain | CyberFundamentals Contribution |
|---|---|
| Risk management | Threat awareness, asset inventory, and vulnerability mitigation |
| Incident handling | Logging, alerting, and backup verification routines |
| Business continuity & recovery | Disaster recovery planning, regular restore testing |
| Supply chain security | Vendor control assessments, network segmentation |
| Policy and governance | Defined security roles, access control policies |
| Training and awareness | Basic cyber hygiene training for staff |
Why this matters for healthcare:
- You can start where you are: Don’t have a CISO? No problem. The Basic level helps you lay the groundwork with minimal resources.
- You won’t over-engineer your defenses: A small outpatient clinic doesn’t need the same setup as a national trauma center. CyberFundamentals respects context (although the “small” package would probably not achieve NIS2 compliance)
- It’s compliance-friendly: Many controls in the framework line up directly with NIS2 expectations. That means less duplication and easier audits.
Bonus benefit: Avoiding checkbox security
Compliance should never mean “just enough to pass an inspection.” By using CyberFundamentals as your base you’re building resilient systems that are harder to break and faster to recover.
If NIS2 is the law of the land, CyberFundamentals is your survival kit. It helps healthcare orgs of all sizes turn good intentions into actual protections, without the bureaucratic overhead.
The Role of Collaboration and Sector-Specific Guidance
Cybersecurity in healthcare isn’t a solo mission. No single hospital, clinic, or healthtech startup can fend off today’s threats alone. Whether it’s a ransomware wave hitting half a continent or a zero-day vulnerability in a medical device vendor, collaboration is now part of survival.
Why collective defense matters in healthcare:
- Threats move fast—faster than most patch cycles. If one hospital sees a new phishing tactic or attack vector, others need to know. Yesterday.
- Many attacks spread laterally through supply chains. A breach at a shared IT provider can impact dozens of organizations overnight.
- Small providers benefit from big providers’ lessons. What a university hospital learns from an incident can protect a regional care center down the road.
Real-world collaborative efforts:
- CERTs and ISACs (Information Sharing and Analysis Centers) dedicated to healthcare, often at national or EU levels, help organizations share intel securely.
- In Belgium, for example, the Cybersecurity for Hospitals Focus Group allows peer hospitals to exchange playbooks, test results, and even simulation scenarios.
- The EU is pushing sector-specific guidance for essential entities—especially in healthcare—so that NIS2 doesn’t feel like a generic IT checklist.
Practical examples of sector-tailored guidance:
- How to isolate infected MRI systems without shutting down the whole radiology network.
- What to communicate to patients and media during a ransomware attack.
- How to handle third-party apps in clinical workflows while maintaining compliance.
What this means for you:
- Join the community: Whether it’s a hospital group, national CSIRT, or even an online peer forum.
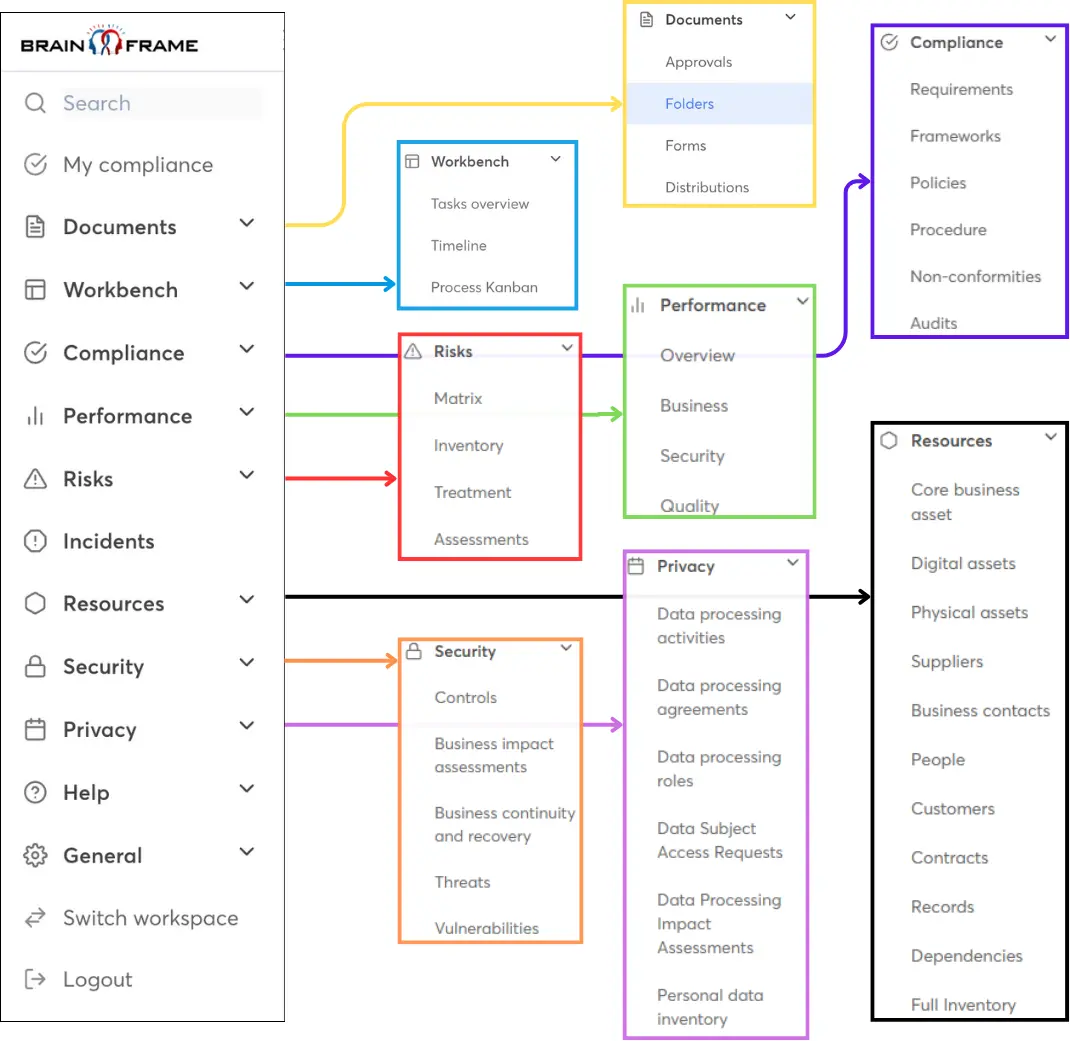
- Don’t reinvent the wheel: Someone has already written the policy template or playbook you need. Borrow, adapt, and improve. Can’t find it? You can reuse directly from Brainframe’s pre-built templates, or let us create it for you with our Policy & Procedure Generator.
- Think beyond IT: Nurses, doctors, and administrative staff all play a role in cyber defense. Make them part of the plan.
Getting Ready – A Checklist for Healthcare Security Leaders
Regulations like NIS2 can feel overwhelming at first glance. But with the right mindset—and a practical framework like CyberFundamentals—you can break the work into manageable steps. The goal isn’t perfection on day one; it’s measurable progress toward better protection, faster response, and smarter governance.
Here’s how to get moving without the panic button.
Step 1: Assess where you stand
- Run a gap analysis against NIS2 requirements, ideally using a readiness checklist tailored for healthcare.
- Evaluate which CyberFundamentals level your organization realistically fits today (Important? Essential?).
- Map your critical systems: EHR, backup systems, connected devices. Know what needs protecting.
Step 2: Prioritize what matters most
- Multifactor authentication (MFA) for clinical systems and remote access? Non-negotiable.
- Offline, tested backups? Absolutely essential.
- Asset inventory and patching plans? Foundational.
- Incident response playbooks? At least one scenario for ransomware, one for data breach.
Start here before diving into encryption policies or third-party audit frameworks.
Step 3: Get leadership on board
- Speak their language: don’t say “threat actors exploited CVE-2023…”—say “a data breach here would delay surgeries and risk patient trust.”
- Present a timeline with phases: Q3 – MFA rollout, Q4 – response drills, Q1 – supplier reviews.
- Tie it back to NIS2 fines, operational risks, and patient safety. That’s your trifecta.
Step 4: Build momentum, not burnout
- Assign roles and owners. Even a small IT team can do more when responsibilities are clearly shared.
- Look for quick wins: patching old Windows servers, removing unused admin accounts, training frontline staff on phishing recognition.
- Don’t aim for ISO certification in one go. Nail the basics, then grow.
This will give you a good chance to build real resilience. The kind that keeps MRI scanners running, patient data private, and doctors focused on saving lives instead of rebooting locked-down systems.
You are not alone!
If you need assistance, don't hesitate to reach out to us. We have a broad network of specialists in Europe that are ready to support your internal teams. Through our Brainframe GRC solution, we can also support you to fully digitalize all the required documentation and processes.